4. The assessment and support of working ability in occupational health care
The patient case of Lauri (duration 7:19)
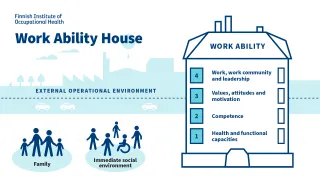
Improving working ability with the Työkykytalo model
The term “working ability” is used to describe a person's ability to work or manage their work-related tasks both in assessing their working ability and improving it. The Työkykytalo model highlights the importance of work and working conditions. The model also considers social issues and focuses on realizing working ability, getting through at work and assessing its conditions. A singular person is considered an active operator in this model. The Työkykytalo model pictures working ability as a four-story house. The base (the first floor of the house) is the physical, psychological, and social functional ability.
Assessing working ability
The assessment of working ability requires knowledge of the demands of working, including the patient’s subjective view of their ability to work, which can be established using self-assessment methods such as the Work Ability Index (WAI) or “Kykyviisari” (the Abilitator). The subjective estimation is complemented by an objective assessment made by occupational health care, which uses assessment methods of physical, psychological, and social functional ability.
When assessing psychological functional ability, the patient is usually interviewed. In addition, methods suitable for charting psychological and cognitive symptoms can be used, for example using ones found in the TOIMIA Functioning Measures Database, such as Beck’s depression quiz, returning to work readiness, the sense of self-efficacy regarding returning to work, and the felt stress.
Physical functional ability is investigated more accurately by an occupational physiotherapist. When charting physical functional ability, methods from the TOIMIA database can be utilized again, for example, the submaximal ergometer test, the squatting test, the grip strength test, the functional balance test, and the upper limb dynamic lift test. These tests are not directly related to working ability, so caution should be taken not to draw hasty conclusions solely based on physical functional ability or the patient’s subjective assessment. When assessing the ability to work, simulations that mimic working tasks can be utilized if conducting the estimation at the worker’s actual place of work is not possible.
The conclusions made from the assessment are added to the patient files, and those made by different professionals are utilized when co-ordinating the patient’s return to work or completing the medical report.
The estimation process of working ability in occupational health care
When a treatment or an operation is made in specialist health care, they also send a referral to occupational health care to assess working ability and its required supporting actions. The referral arrives at the OHC and is delivered to the case manager, who contacts the patient and directs them to required professionals to assess working ability in the planned order, considering, for example, the required information from different medical fields in order to complete the medical report.
Working ability and its supporting actions
A multiprofessional team makes assessments of working ability
Estimations in occupational health care are made by a multiprofessional team. The planning is made on a case-by-case basis in terms of which occupational group representatives are a part of the assessment process and who keeps in contact with the patient and their workplace. Practically speaking, appointments are booked with different professionals while considering the unique recovery process of each patient.
When assessing the patient’s need for support regarding their working ability and making an estimation of when they can return to work, each professional is required to not only have an estimate of the patient’s individual needs and their recovery prognosis, but also have the knowledge of the requirements of their work, the supporting models used at their place of work, and the opportunities of the social security system when helping the patient return to work.
The multiprofessional team of occupational health care usually consists of:
Returning to work
Based on the assessment of work ability, the patient's timely return to work is planned, utilizing, for example, job modification possibilities or the substitute work model. Job modification is used to adjust the patient's work tasks to match his work ability in situations where the symptoms limit work to some extent. Substitute work is used in situations where the patient's symptoms prevent one's own work.
Measures for supporting returning to work
Monitoring working ability
An occupational health care staff member is assigned to monitor the patient’s ability to work and their need for supporting actions both before and after they return to work. The monitoring can be implemented by various professionals, either as remote meetings or as physical appointments.
Occupational health negotiation
The representative of the employer must identify which opportunities exist in the workplace to make changes to work and work arrangements, and what work-related requirements are present in different jobs and their potential replacements.
The employee needs to make sure that the occupational health care can access all the patient files related to the issue at hand (Kanta rights). They should also spend some time thinking what would support their work and functional ability and returning to work, and prepare to discuss issues related to managing their work. The representative of the occupational health care and the employee must have a discussion before the negotiation in which they decide which issues the employee does not wish to bring up in the negotiation and which issues should be brought up.
Occupational health care must assign a person who invites all the participants of the negotiation to a meeting and makes sure that the occupational health doctor attending has all the correct information present at the negotiation, such as:
- Current information of the employee’s working ability and their recovery prognosis
- Information related to the factors of returning to work and the correct timetables
- Information written in the plan of action made in occupational health care regarding the models of early support in the workplace
The conclusions of the negotiation are consolidated into a memo, which will contain the issues that are agreed upon by the participants. A monitoring meeting can be held if deemed necessary. The occupational health negotiation is usually held in a way where all parties are physically present, but it can also be held remotely.
